David Hutton, University of Michigan
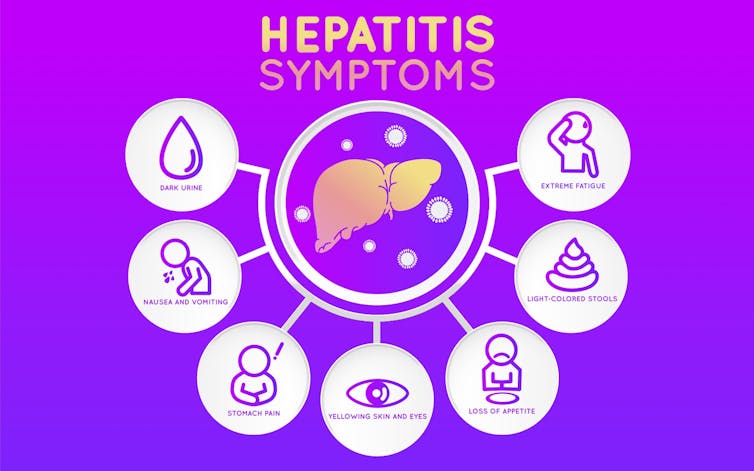
Very few people know about hepatitis B, the so-called silent killer, and the billions of dollars it costs the U.S. health care system. The hepatitis B virus can cause chronic infection that is usually asymptomatic for decades until it leads to costly, debilitating liver cirrhosis or liver cancer.
The World Health Organization is appealing to countries to significantly increase screening and treatment of hepatitis B to reduce hepatitis deaths by 65 percent. But this is costly and the U.S. has other competing health priorities. Is it worth our time and effort to try to achieve the goals set by WHO? My colleagues and I recently addressed the question in the journal Health Affairs and concluded it is a valuable public health initiative that could potentially save almost half a billion dollars in the long run.
I am a public health researcher interested in how we can spend our health care dollars wisely to boost the health of the population. I was inspired to focus on hepatitis B health policy through Dr. Sam So, a hepatitis B advocate at Stanford University who is trying to raise awareness of this serious, under-recognized disease. We teamed up with my co-author Dr. Mehlika Toy to examine hepatitis B policy.
Kateryna Kon/shutterstock.com
The goal of our research team was to calculate whether it would be cost-effective for U.S. health practitioners to take up and execute WHO’s challenge.
A stealthy virus
Over a million people in the U.S. are estimated to be living with chronic hepatitis B infection, but only about a third know they have the disease and only about 15 percent of those are receiving treatment.
Hepatitis B is caused by a virus that leads to liver disease and is transmitted during childbirth or by blood, semen or other body fluid. Fortunately, most Americans born in the last 30 years have been vaccinated and are protected. But, for those born in other countries, particularly in Asia or Africa, the risk of having a chronic infection is high.
A majority of those in the U.S. with chronic hepatitis B are immigrants. The good news is this disease can be treated with long-term antiviral drug therapy, dramatically reducing risks of cirrhosis and liver cancer, which are much more expensive to treat.
Since hepatitis B progression takes decades, my group built a mathematical model of immigration and hepatitis B disease progression to simulate what will happen when Asian and African immigrants to the U.S. wait until they became ill before seeking treatment. We then compared what their health and costs would look like if we met WHO’s specific goals and diagnosed 90 percent and treated 80 percent of immigrants.
By iLoveCoffeeDesign/Shutterstock.com
Herculean effort to screen
In order to reach these targets, the U.S. would have to give a blood test to 14 million foreign-born individuals from Asia and Africa over the next seven to 12 years.
We included the additional costs required for outreach to these marginalized populations that are poorly integrated into the U.S. health care system. We estimate that insurers and patients in the U.S. would spend between US$700 and $800 million over the next 50 years screening people for hepatitis B. Although that sounds like a lot of money, dramatic increases in screening and treatment would prevent between about 80,000 and 100,000 cases of cirrhosis, 50,000 and 60,000 cases of liver cancer, and 80,000 to 100,000 hepatitis B-related deaths over the next 50 years.
The savings from preventing cirrhosis and liver cancer could pay for the costs of screening and treatment if they were achieved by 2025. If the U.S. could achieve those goals by 2025, we estimate the U.S. health care system would save $1.2 billion in hepatitis B treatment costs. When we account for the screening costs to achieve this, we would see net savings of about $400 million to patients and insurance companies.
Public health value of screening and treatment

FF2011/Wikimedia Commons, CC BY-SA
In contrast, when my colleagues and I examined this policy a decade ago, we determined that screening and treating adult Asian and Pacific Islanders would not save money, but would instead cost between $30,000 and $40,000 per year of healthy life gained.
So, why is hepatitis B screening and treatment so much more valuable now? In the last year, there have been dramatic reductions in the price of antiviral treatment because highly effective generics have reached the market. Treatments that used to cost many hundreds or even thousands of dollars a month are now only $115 per month. So now the analysis tips heavily in favor of screening and treatment.
These findings are unique and significant because many prevention interventions do not save money. A 2008 study of the academic literature on cost-effectiveness found that fewer than 20 percent of the prevention interventions led to cost savings.
![]() Of course, our health care system does not exist solely to save costs. Improving quality and length of life are important, but the fact that most studies are not cost-saving illustrates how uncommon our results are. It also highlights that increasing screening and treatment of hepatitis B ought to be prioritized.
Of course, our health care system does not exist solely to save costs. Improving quality and length of life are important, but the fact that most studies are not cost-saving illustrates how uncommon our results are. It also highlights that increasing screening and treatment of hepatitis B ought to be prioritized.
David Hutton, Associate Professor of Health Management and Policy , University of Michigan
This article was originally published on The Conversation. Read the original article.